Unraveling the Secrets of Cancer Drug Resistance: A Glimpse into the Future of Cancer Treatment
Cancer, a scourge that has touched countless lives, not only inflicts physical and emotional pain but also poses a significant financial burden. The cost of treating cancer can soar into several lakh rupees, depending on the type of cancer, available treatment options, and whether the treatment is administered in a public or private setting. This financial strain, coupled with the physical and emotional toll cancer takes on individuals and their families, makes the battle against cancer an arduous one.
One of the most challenging aspects of treating cancer is its ability to rebound, often following a period of remission. This resurgence can be attributed to a small group of cancer cells that exhibit resistance to anti-cancer drugs. These resilient cells manage to survive and even thrive in the face of potent treatments. To improve the odds of defeating cancer for good, it is imperative to understand the mechanisms behind this drug resistance.
A recent study, published in Cell Reports on September 20, has shed light on a crucial aspect of drug resistance in cancer. Researchers from the Netherlands Cancer Institute explored the resistance of certain cancer cells to a drug known as Taxol. What they discovered could revolutionize the way we approach cancer treatment.
The Challenge for Oncologists
Cancer cells are notorious for their rapid, uncontrolled division. Anti-cancer drugs, also known as chemotherapeutic agents, work by halting or obstructing this unbridled proliferation. When a cancer cell's division is arrested, it typically responds by initiating programmed cell death, a process known as apoptosis. This response ensures that the cancer cells are eliminated while sparing nearby non-cancerous cells that aren't actively dividing.
However, this precision comes at a price. Chemotherapy can cause collateral damage to tissues with a significant number of normally dividing non-cancerous cells. These include cells in the digestive tract, bone marrow, and hair follicles. The result is painful side effects such as oral and gut inflammation, nausea, diarrhea, anemia, and hair loss. Oncologists face the daunting challenge of finding the right drug dosage that effectively eradicates cancer cells while minimizing unbearable side effects for the patient.
Antibody-Drug Conjugates: A Ray of Hope
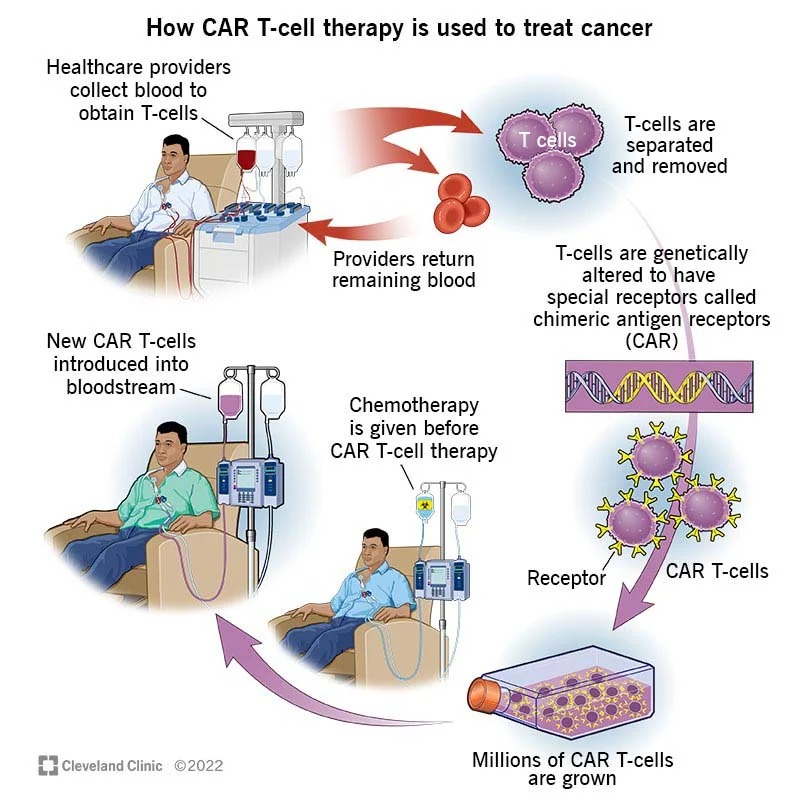
To address this challenge, researchers have developed antibody-drug conjugates (ADCs) against certain cancers. ADCs are drugs attached to antibodies that specifically recognize proteins found predominantly on cancer cells. These antibodies act as guides, directing the chemotherapeutic drug to the cancer cells while sparing non-cancerous ones.
The Role of P-gp: A Roadblock to Treatment
However, a subset of cancer cells can still evade the impact of anti-cancer drugs. This resistance is often attributed to elevated levels of a protein called P-glycoprotein (P-gp). P-gp acts as a pump within the cell, expelling toxic compounds. In cells that overproduce P-gp, this protein efficiently removes toxins, including chemotherapeutic agents, preventing them from accumulating to levels that would trigger apoptosis. This allows cancer cells to survive and potentially lead to a cancer relapse.
Cracking the Code of Resistance
The recent study in Cell Reports delves into the resistance of certain cancer cells to Taxol, a drug widely used in cancer treatment. The research used cells from the human eye retinal pigment epithelium as a model to understand the resistance mechanism. The study uncovered that a cell's sensitivity to Taxol and its ability to resist the drug is related to the location of a specific gene called ABCB1 within the cell's nucleus.
The nucleus of a cell contains DNA and associated proteins. Genes are segments of DNA, and when a gene is expressed, it means the cell can use it as a template to form RNA molecules. RNA carries out many of the same functions as DNA, with the essential difference being that RNA enters the cytoplasm – the rest of the cell – where it instructs the cellular machinery on how to build the protein encoded by the gene.
In cells that were sensitive to Taxol, the ABCB1 gene was found close to the nuclear envelope. In resistant cells, this gene had moved further inside the nucleus. This location change led to a 100-fold increase in the amount of RNA corresponding to the ABCB1 gene in resistant cells compared to sensitive ones. The RNA was used to create the P-glycoprotein efflux pump, which was responsible for Taxol resistance.
Unraveling the Role of LBR
To understand what kept the ABCB1 gene attached to the nuclear envelope, the researchers deactivated different genes to observe the impact on the proteins that form the nuclear envelope. They identified a protein called lamin B receptor (LBR) that seemed to be responsible for tethering the ABCB1 gene. In cells without LBR, the ABCB1 gene could be activated when exposed to Taxol. When the gene used to make LBR was deleted, cells didn't immediately increase the expression of ABCB1. It was only when exposed to Taxol that the expression surged.
The study also looked at the effect of depleting LBR in various types of cancer cells. The results were intriguing: lung cancer cells, already expressing a high degree of ABCB1 RNA, didn't become more resistant when LBR was removed. On the other hand, breast cancer cells exhibited increased Taxol resistance when LBR was depleted, but this effect wasn't observed in head and neck cancer cells.
Why Different Cancers Respond Differently
The differential response of various cancer types to LBR depletion might be understood with an analogy. Imagine drying clothes in a bathroom with limited options for hanging them: hooks, towel rods, or a ledge. If the bathroom only has a few hooks, the risk of clothes piling up and falling is high. However, with multiple options, like towel rods and a ledge, the risk decreases.
Similarly, breast cancer cells might have depended more on LBR to tether genes to the nuclear envelope than other cancer cell types. This variation in response highlights the complexity of gene regulation and silencing within different cancer cells.
A Glimpse into the Future
Understanding the diverse ways in which cancer cells express or silence genes can open new avenues for research and treatment. This study offers a promising path to ensuring that anti-cancer drugs remain potent and efficient, enabling patients to recover faster and with fewer side effects. As researchers continue to decipher the intricacies of cancer drug resistance, we inch closer to a future where cancer treatment is more effective and less taxing on patients.